Release date: 2018-02-24
Recently, scientists at the Washington University School of Medicine in St. Louis have transformed skin cells from patients with Huntington's disease into brain cell types affected by the disease.
The researchers say that the large number of neurons acquired will serve as a new tool for studying this degenerative and ultimately fatal neurological disease.
The study, published in the February 5 issue of Nature Neuroscience, showed that nerve cells directly transformed from the skin cells of patients showed "symptoms" of the disease, including DNA damage, mitochondrial dysfunction. And cell death. Correcting genes for dysfunction in these reprogrammed neurons prevents the characteristic cell death of Huntington's disease.
Huntington's disease is a genetic disorder that causes cognitive decline and involuntary muscle movement. These symptoms usually appear in patients 30-50 years of age and worsen over time. The average survival time of patients after the onset of symptoms is approximately 20 years.
Dr. Andrew S. Yoo (PhD), a senior author and assistant professor of developmental biology, pointed out: “This is a powerful tool for exploring the causes of specific brain cells that carry disease-related mutations that decay over time and eventually die. In theory, We can model the progression of the disease by reprogramming the skin cells of patients of different ages (including before the onset of symptoms). If drugs or compounds may help these patients, we can first test them in this system."
Research on Huntington's disease and other hereditary encephalopathy is challenging because it is difficult to obtain neuronal specimens from living patients. The good news is that scientists have discovered ways to convert skin cells into brain cells.
Skin cells are readily available and share the same genetic map and pathogenic mutations as brain cells. Researchers, including the first author and postdoctoral research assistant Dr. Matheus Victor (PhD), set out to produce neurons that mimic adult patients to model the pathogenesis and development of Huntington's disease. They achieved this goal through the direct conversion method developed.
This method allows skin cells to skip the stem cell stage when reprogrammed into neurons. After the stem cell stage, the developmental clock will be reset to the embryonic stage, which will erase the age-related effects of the disease. But directly reprogrammed neurons retain age and problems associated with adult-born Huntington's disease, Dr. Yoo and colleagues say.
In direct reprogramming, researchers exposed adult skin cells to a mixture of specific signaling molecules that have been found in previous studies to convert healthy skin cells directly into so-called medium spiny neurons ( Medium spiny neurons) specific brain cells without intermediate steps. The "signal cocktail" repackages the DNA, folding the instructions of the skin cells and unfolding the neurons. The reprogrammed medium-sized spiny neurons obtained by this method retain the age course of the patient as well as age-related disease symptoms.
Although other neuronal types are also affected by Huntington's disease, medium-sized spiny neurons are the first to bear the brunt. The genetic error that causes the disease can cause the critical protein Huntigtin to be deformed and not working properly. As a result, dysfunctional proteins accumulate and eventually kill cells through certain unknown events. Since neuronal death can be re-described in direct reprogramming neurons, Yoo points out that the new technology provides a way to study the details of how potential therapies, including those being tested in clinical trials, can rescue medium-sized spiny neurons.
Yoo and colleagues identified another important protein when it comes to understanding the details of how the disease develops to cause cell death. This protein, known as SP9, is known to be essential for normal mid-sized spiny neurons, but has not previously been associated with Huntington's disease. The researchers found that SP9 protein was significantly less in medium-sized spiny neurons transformed from Huntington's disease. They conducted an experiment in which SP9 was administered back to diseased neurons and found to reduce cell death to levels similar to healthy control cells.
Yoo said: "We want to understand what drives disease over time, and most neurodegenerative diseases worsen over time, so this modeling approach may be applied to other diseases. This technology allows us to capture different diseases. The characteristics of time. This is important for understanding the problems that arise and for finding ways to stop them."
Source: China's rare disease
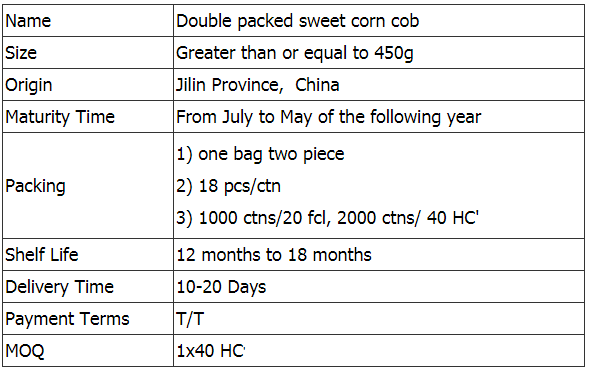
Fresh Double Packed Sweet Corn
Jilin Province Agricultural Sister-in-law Food Co., Ltd. was establishe in 2012, is a diversified company based on corn food's research and development, production, and sales. Through several years' rapid development and innovation, Nongsao gradually became a modern company of certain scale.
Jilin Province Agricultural Sister-in-law Food Co., Ltd. is located in Gongzhuling City, Jilin Province, one of the three golden corn belts in the world. The corn belt in Jilin Province is well suited for corn growing conditions, and more than 60% of the arable land is suitable for corn growing, so the total corn production and commercial grain rate in Jilin Province has been the first in China. Jilin Province is the main corn producing region in China and the main grain exporting province of the country.
Unlike other regions, Jilin has a cold-temperate humid and semi-humid climate. The frost-free period is short throughout the year, about 130-170 days, and the annual precipitation reaches 400-800. July-September is the peak period of precipitation, which is more suitable.


If you have any questions, please contact us directly. Welcome to visit our factory, if you have any questions, please email us directly.
Local Sweet Corn,Sweet Corn For Diet,Sweet Maize Cob,Packed Sweet Corn
Jilin Province Argricultural Sister-in-law Food Co., Ltd. , https://www.nongsaocorn.com